Psoriatic Arthritis
Encinitas, CA patients find effective relief from psoriatic arthritis
Seaside Rheumatology is located in Encinitas CA, providing quality rheumatological care for patients throughout the region. This includes a number of advanced treatment options for psoriatic arthritis (PsA).
What is psoriatic arthritis?
Psoriasis is an autoimmune disorder, which is generally known for its effects on the skin. It is characterized by raised, reddish skin lesions, often covered in silvery scales. About one in four psoriasis patients also have psoriatic arthritis, which is an inflammatory condition affecting the joints but also surrounding tendons and ligaments. Psoriatic arthritis involves swelling, pain, tenderness, and stiffness of not only the joint but also the ligaments and tendons.
Psoriatic arthritis is an inflammatory arthropathy, which means that it is characterized by inflammation of the joints. It can affect the spine, and in some cases is a contributing factor to enthesitis (a type of inflammation affecting the joint cap, ligament, or tendon). Therefore, psoriatic arthritis is sometimes classified as a seronegative spondyloarthropathy, meaning a joint disease of the spine, which is negative for rheumatoid factor (an antibody present in rheumatoid arthritis).
Risk factors and diagnosis
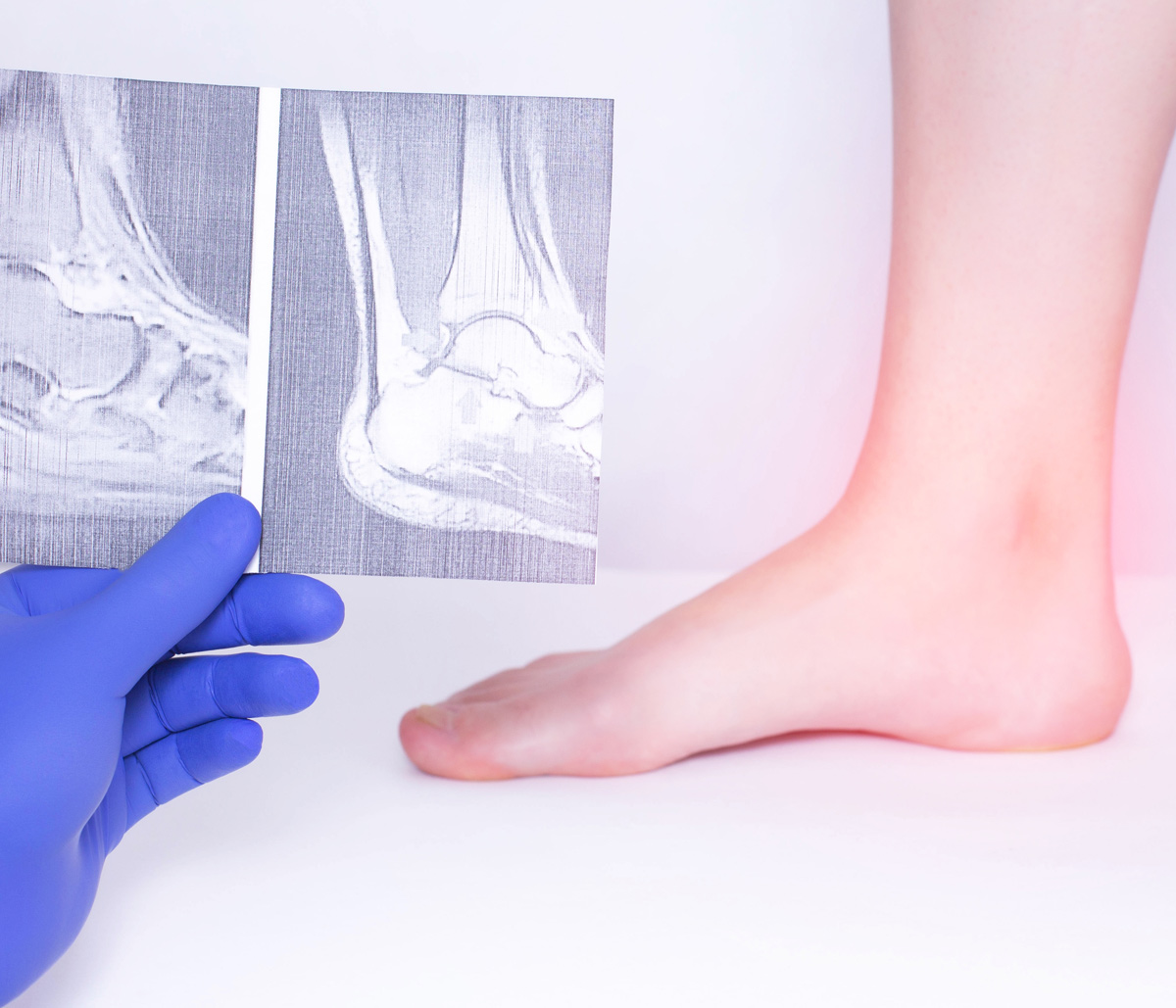
There isn’t a definitive test for psoriatic arthritis. Diagnosis of the condition is based on evaluation of multiple factors, including physician examination, patient’s medical history, laboratory testing, and imaging. One of the preferred tools for diagnosing psoriatic arthritis, especially in the early stages, is musculoskeletal ultrasound imaging.
Gender is not a risk factor for psoriatic arthritis, males and females are equally affected.
Increased risk of psoriatic arthritis has been associated with the presence of human leukocyte antigen B27 (HLA-B27), which is a protein on white blood cells’ surface.
The condition most often develops between the ages of 30 and 50, though it can happen at any age.
Skin symptoms typically appear about a decade before the onset of psoriatic arthritis. However, in 14 to 21 percent of cases, arthritis symptoms precede skin problems.
In about 30 to 40 percent of psoriatic arthritis patients, there is some intestinal involvement, such as the presence of Crohn’s disease, irritable bowel syndrome (IBS) or ulcerative colitis.
Recent studies have shown a prevalence of genes associated with celiac disease, gluten intolerance, or inflammatory bowel diseases in people with psoriatic arthritis and psoriasis.
What is Psoriatic Arthritis? - Dr. Peter Lloyd

Typically patients with psoriatic arthritis will first have the skin condition known as Psoriasis. Those select small groups of patients will develop psoriatic arthritis before they develop psoriasis.
Psoriatic arthritis is an inflammatory Arthritis, that can affect any age group.
It’s an inflammatory condition, meaning that it has nothing to do with age or age-related arthritis. It can happen with young patients or old patients.
Psoriatic arthritis patients have joint pain, swelling, and stiffness in both the peripheral joints. For example, the wrists, the fingers, the elbows, etc.
But also in the axial system, the spine. They can have stiffness and pain in the lower region of the spine and the neck. So basically, any joint can be involved.
Symptoms and subtypes
The severity of psoriatic arthritis can range from mild and nondestructive to severe and erosive. Additionally, there are several subsets of the condition, including:
- Monoarthritis – Inflammation of an individual joint (usually affects larger joints)
- Distal interphalangeal arthritis – Affecting the knuckles nearest the tips of fingers
- Spondyloarthritis – Affecting the joints as well as areas where ligaments and tendons attach to the bone
- Symmetrical deforming polyarthropathy – Symptoms very similar to those of rheumatoid arthritis.
If psoriatic arthritis is not treated, persistent inflammation can develop along with joint deformation. It can become debilitating, severely limiting the patient’s physical activity. The effects may include:
Often, the articular wear patterns of joints may change over time or begin to overlap.
Enthesitis (inflammation of ligament or tendon connective sites) may occur in any area of the body, but it is most common at the plantar fascia insertion point (bottom of the foot), Achilles tendon (heel), spine, ribs, and pelvis.
Dactylitis, or “sausage digit,” is severe inflammation of fingers or toes, which commonly occurs in psoriatic arthritis patients.
The condition can also affect the eyes, with conditions such as urethritis, iritis, or conjunctivitis frequently seen in psoriatic arthritis patients.
It can lead to damage or joint deformity, including asymmetric sacroiliitis, nonmarginal asymmetric syndesmophytes, spur formation, arthritis mutilans, the presence of pencil-in-cup deformity, and bone erosion.
Treating psoriatic arthritis
Much progress has been made in recent years, furthering scientific understanding the epidemiological and clinical characteristics of psoriatic arthritis, and defining its immunologic and genetic associations. Most significantly, many advances have been made in the area of targeted biologic or systemic psoriatic arthritis treatments.
Traditional therapy includes non-steroidal anti-inflammatory drugs (NSAIDs), disease modifying drugs (DMARDs), biologics and phosphodiesterase 4 inhibitors.
NSAIDS, including ibuprofen, naproxen, diclofenac, indomethacin, and other similar drugs provide rapid relief for pain and acute inflammation. NSAIDs help with symptomatic relief, but they do not alter the disease course or prevent disease progression.
DMARDs, including methotrexate, sulfasalazine, cyclosporine, leflunomide, hydroxychloroquine, azathioprine and methotrexate are potent anti-inflammatory drugs with delayed mode of action (time to produce intended effect). Traditionally, DMARDs have been used to treat psoriatic arthritis affecting mainly peripheral but not the axial (spine, sacroiliac) joints.
Biologics, tumor necrosis factor-alpha blockers including; etanercept (Enbrel ®), adalimumab (Humira ®), golimumab (Simponi ®), certolizumab (Cimzia ®) and infliximab (Remicade ®). Others include Interleukin 12/23 blocker ustekinumab (Stelara ®)and interleukin 17-A blocker secukinumab (Cosentyx ®) and ixekizumab (Taltz ®). These medications are taken by injection or IV infusion.
Other: phosphodiesterase 4 inhibitor apremilast (Otezla ®) is an oral medication.
Integrative therapy includes dietary modifications and food supplements as treatment.
The most beneficial generic dietary interventions in psoriatic arthritis include a combination of gluten-free, dairy-free, egg-free and soy-free diet. Some food supplements and herbs utilized to treat psoriatic arthritis include: omega-3 polyunsaturated fatty acids, black currant seed oil, Boswellia, turmeric, devil’s claw, Yucca schidigera, sea cucumber extract, pro- and prebiotics and Oregon grape.
Relief is a phone call away
Without appropriate treatment, psoriatic arthritis can progress to the point of becoming debilitating, with long-term bone or joint damage. If you have been diagnosed with this condition, or if you experience any symptoms, please call Seaside Rheumatology and Wellness Center, and schedule a consultation with Dr. Lloyd right away.